This post continues the previous one’s focus on the just announced registering of all TB patients nationally through the UID/Aadhaar program, as a disease control measure for a national population increasingly conceived of as migratory or “deterritorialized.” It is also a response to Peggy Trawick’s comment on that earlier post suggesting that programs like UID miss the point and that tackling TB must focus on the fundamental conditions of the physical milieus in which people live.

Drug-resistant TB patient in Mumbai (Deccan Chronicle photo)
It begins by engaging a similar article to the one discussed yesterday, from the Asian Age newspaper of 7 July 2012. It then develops a reference to the disastrous “Mumbai episode,” reading a recent article in the Lancet.
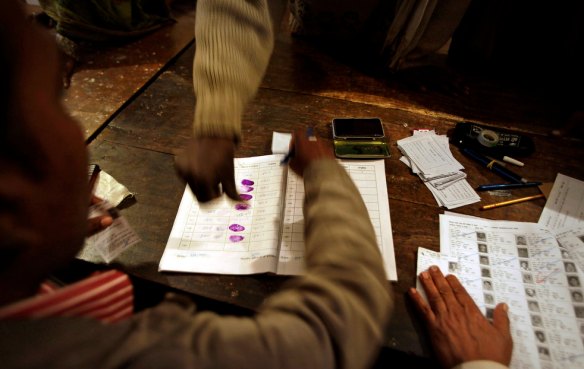
TB patients to get UID number
Starting July 15, patients suffering from tuberculosis will be given a unique identification number by the state government, to keep tab on the spread of the disease. A specialised software will connect all facilities treating tuberculosis patients, to avoid duplication of cases. Already 60 data entry operators working in the government, have been trained to use the specialised software, where the data of each and every TB patient in the state will be uploaded. “After the Mumbai episode, we had proposed a common software across all states. The government of India has already designed a common software for all states, in which the data of each TB patient will be uploaded,” said Dr Pradeep Gaikwad, joint director, tuberculosis and leprosy…
According to state health officials, the software will help the state trace the patient, even if he migrates to other states or other parts of the state. Having common data will also help avoid duplication of cases. “The major reason for the rise in resistant tuberculosis is because of defaulter patients, who stop their treatment mid-way. If a patient goes to another state, he/she can give his unique identification number to the doctor; this will help the doctor understand his/her case history and give the required medication to him/her,” Mr Gaikwad added. The patient’s contact number, Aadhar card number and other medical details will also be uploaded in the software, so that doctors can trace him/her, even if he/she stops coming to the hospital. Mr Gaikwad, however, warned that owing to the active case finding intervention, the number of tuberculosis cases in the state could rise.
According to the state health department records, of 1.35 lakh tuberculosis patients, 25 per cent fall under the multi-drug-resistant tuberculosis [MDR-TB] category.
This article offers a clearer rationale for the new program than the earlier article: centrally at stake is the tracing of TB patients to ensure that they complete the course of their medication. UID/Aadhaar becomes an extension of DOT, Directly Observed Therapy, a massive up-scaling of a surveillance intervention focused on local knowledge and intimate observation to ensure drug regime adherence. This tracing includes not only migration but also non-compliance in place, as it were.
Of note is the relation of the Aadhaar/UID number to residence information, a much debated feature of its data set. Like the banking and finance industries, the public health establishment requires location-specific data of Aadhaar. But one of the promises of UID early on was its deterritorialization, that is, its naming and characterizing an individual not through his or her native place or father’s village or town but through mobile biometrics. Implicit in the deterritorialization was an understanding of corruption (say, the cut a local official may exact of someone’s pension) that presumes that mobile identity allows individuals to evade this intimate and localized corruption.
With TB, as with finance, trust however depends on the ability to locate the registrant. UID promises the doctor that she or he can find the UID subject using the data encoded and linked to his or her UID number. This spatial legibility is tied both to data and to use. For those who want UID to include spatial data, actual residence is included and available to those agencies with access to UID information. But UID number use itself produces a trace of location, much as a credit card would. To the extent more and more “minimal entitlements” from ration cards to employment guarantees to more and more state/private/NGO outlays are linked to UID, life itself becomes impossible without one showing up on a database somewhere in India or through its consular extensions.
That the public health state can trust locational data is critical as it must respond to its own massive failure, here the somewhat vague reference to the “Mumbai episode.”
For now, I am assuming that this episode is the much reported finding, early in 2012, that several cases of entirely multi-drug resistant tuberculosis had been found in Mumbai. Here is the Lancet of 21 January 2012:
India reports cases of totally drug-resistant tuberculosis
Samuel Loewenberg
Mismanagement of tuberculosis in Mumbai has led to the emergence of India’s first known cases of a totally drug-resistant form of the disease, say doctors. Samuel Loewenberg reports.
Researchers in Mumbai have identified 12 patients with a virulent strain of tuberculosis that seems to be resistant to all known treatments. The cases of so-called totally drug-resistant tuberculosis (TDR-TB) have been detected in the city in the past 3 months. Worldwide, the only other episodes of TDR-TB reported were in Iran in 2009 and Italy in 2007.
What then follows is a social diagnosis: a miserable state system drives persons to mostly untrained clinicians whose prescription patterns drive increased drug resistance: the state fails entirely either to regulate the latter or to address the failures of the state system.
“Basically, it is a failure of public health, and that has to be accepted in this country”, said Zarir F Udwadia, who has been treating the patients at the P D Hinduja National Hospital and Medical Research Centre, and who, along with colleagues, described four of the cases in a letter published online in Clinical Infectious Diseases. “The public doctors and private doctors are equally to blame”, he said. The city’s health officials reject these charges. “State TB care and health care in Mumbai is excellent”, Anil Bandiwadekar, the Executive Health Officer of the Public Health Department of the Municipal Corporation of Greater Mumbai, the city’s governing body told The Lancet.
Government health officials attribute the problems with drug-resistant tuberculosis to the city’s unregulated private doctors who prescribe inappropriate drugs. Privately, some senior officials acknowledge that much of the public have a negative perception of government-run health facilities, due to long waiting periods, rude treatment, and the stigma associated with tuberculosis. The result is that many infected people avoid the government tuberculosis programme and seek relief from private doctors, only some of whom have medical training. The government says that it is considering regulating tuberculosis drugs, but it has not yet taken action.
Mumbai would seem to be a prime breeding ground for drug-resistant infections. The city, home to more than 12 million people, is beset by poverty, overcrowding, and harsh living conditions.
Udwadia says that although the DOTS (Directly Observed Therapy, Short Course) programme has generally been successful for people with normal tuberculosis who do access it, for those with drug-resistant tuberculosis, it causes more than 8 months of delay as people are forced to go through standard treatments before they are diagnosed. All the time, they are generating further resistance.
The article concludes again stressing the failure of administrative capacity and political will, given the cost of treating MDR-TB, and uses the language of caste to characterize the forms of triage.
Presently, there are only 171 people enrolled in the DOTS-plus programme that has been in effect in Mumbai since 2010 to treat drug-resistant tuberculosis, according to the office of Bandiwadekar. Tuberculosis was estimated to have accounted for at least 15% of the deaths in Mumbai in 2010. India has one of the world’s highest burdens of drug-resistant tuberculosis, (around 100 000 people), according to WHO. The failure of the government to provide treatment for all of these patients is due to the cost—about US$4000 per patient, a high cost for India, which spends only $45 per head on health care. Udwadia says that the government passes its actions off as “health policy real politik”, which in effect means it ignores most of the patients with drug-resistant tuberculosis. “They have become the untouchables of the Indian medical system”, he said.
In fact, health centres and hospitals could be a contributor to the growth in resistance, said Nerges Mistry, the director of the Foundation for Medical Research in Mumbai. There is “poor infection control at most of these settings”, said Mistry, and people with resistant tuberculosis could well be infecting patients with a regular tuberculosis infection. A 5-year study done by the Foundation with the Wellcome Trust found that most patients were resistant to two or three of the first-line drugs, and some to all four. The city could have as many as 3500 cases of multidrug-resistant tuberculosis (MDR-TB) each year, but lacks the laboratory infrastructure in the public system to identify and confirm the diagnosis, said Mistry.
Exposure to MDR-TB is intensified in the city’s giant slums, described here as “notorious.”
Meanwhile, the patients with TDR-TB are walking the streets. Udwadia says that isolation is not practical due to cost and lack of hospital beds. He notes that four of the patients come from Dharavi, a notorious Mumbai slum with a population of 2·5 million people.
So far, three of the TDR-TB patients have died, one of them after lung surgery. One of the patients has passed on her infection to her daughter. Udwadia is trying any treatment he thinks might work. This includes a double-dose isoniazid, the harsh antibiotic linezolid, the anti-leprosy drug clofazamine, the anti-psychotic drug thioridazine, and meropenem and clavunate, which reportedly had some effect on tuberculosis in mice. “We are clutching at straws here”, he admits.
In this context, how to make sense of the turn to Aadhaar, to the new promise of Big Data? What is not addressed is the state’s failure, assuming the arguably inflationary language of the Lancet piece is acccurate, to enroll most persons with MDR-TB or to regulate the conditions of common treatment. Rather, those few persons already in the MDR-TB treatment pipline are to be more effectively surveilled through the UID number.
Or is there a more sustained argument to be made for the utility of UID. given this double failure, of routine TB treatment and of the enrollment of most persons with MDR-TB in treatment?